
We compared 3 models: (1) random forest (2) logistic regression and (3) Hakim model. FN patients who were transferred to the intensive care (TIC) had higher temperature and higher incidence of hypotension at presentation compared to FN patients who didn’t have TIC. Patients who had BSI had higher maximum temperature, higher rates of prior BSI and higher incidence of hypotension at time of presentation compared with patients who did not have BSI. The most common oncologic diagnosis with FN was acute lymphoblastic leukemia (ALL), and the highest rate of BSI was in patients with AML. BSI was diagnosed in 106 (21%) and TIC occurred in 56 (10.6%) episodes.

A total of 505 FN episodes (FNEs) were identified in 230 patients. Performance was assessed using area under the receiver operating characteristic curve (AUC) metrics. Prediction models were built for both outcomes using logistic regression and random forest and compared with Hakim model.
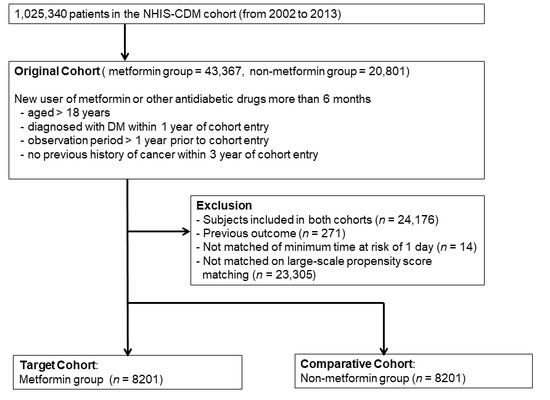
Data were divided into independent derivation (2009–2014) and prospective validation (2015–2016) cohorts. Predictor variables include demographics, clinical, and laboratory measures on initial presentation for FN. The secondary outcome was transfer to intensive care (TIC) within 14 days of FN onset. The primary outcome was onset of BSI, as determined by positive blood culture within 7 days of onset of FN. We excluded stem cell transplant recipients who developed FN after transplant and febrile non-neutropenic episodes. We conducted an observational cohort analysis of pediatric and adolescent cancer patients younger than 24 years admitted for fever and chemotherapy-induced neutropenia over a 7-year period. Our goal in this study was to develop a model for predicting blood stream infection (BSI) and transfer to intensive care (TIC) at time of presentation in pediatric cancer patients with FN.
Febrile neutropenia (FN) is a common condition in children receiving chemotherapy.


 0 kommentar(er)
0 kommentar(er)
